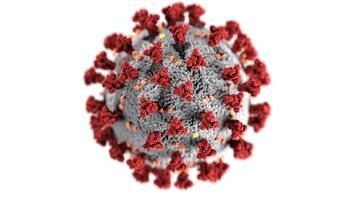
Coronavirus: could it be burning out after 20% of a population is infected?
More than half a million people have died from COVID-19 globally. It is a major tragedy, but perhaps not on the scale some initially feared. And there are finally signs that the pandemic is shuddering in places, as if its engine is running out of fuel. This has encouraged many governments to relinquish lockdowns and allow everyday life to restart, albeit gingerly. The spread of SARS-CoV-2 has been difficult to predict and understand. On the Diamond Princess cruise ship, for example, where the virus is likely to have spread relatively freely through the air-conditioning system linking cabins, only 20% of passengers and crew were infected. Data from military ships and cities such as Stockholm, New York and London also suggest that infections have been around 20% – much lower than earlier mathematical models suggested. This has led to speculation about whether a population can achieve some sort of immunity to the virus with as little as 20% infected – a proportion well below the widely accepted herd immunity threshold (60-70%). The Swedish public health authority announced in late April that the capital city, Stockholm, was “showing signs of herd immunity” – estimating that about half its population had been infected. The authority had to backtrack two weeks later, however, when the results of their own antibody study revealed just 7.3% had been infected. But the number of deaths and infections in Stockholm is falling rather than increasing – despite the fact that Sweden hasn’t enforced a lockdown. Hopes that the COVID-19 pandemic may end sooner than initially feared have been fuelled by speculation about “immunological dark matter”, a type of pre-existing immunity that can’t be detected with SARS-CoV-2 antibody tests. Antibodies are produced by the body’s B-cells in response to a specific virus. Dark matter, however, involves a feature of the innate immune system termed “T-cell mediated immunity”. T-cells are produced by the thymus and when they encounter the molecules that combat viruses, known as antigens, they become programmed to fight the same or similar viruses in the future. Studies show that people infected with SARS-CoV-2 indeed have T-cells that are programmed to fight this virus. Surprisingly, people never infected also harbour protective T-cells, probably because they have been exposed to other coronaviruses. This may lead to some level of protection against the virus – potentially explaining why some outbreaks seem to burn out well below the anticipated herd immunity threshold. Young people and those with mild infections are more likely to have a T-cell response than old people – we know that the reservoir of programmable T-cells declines with age. In many countries and regions that have had very few COVID-19 cases, hotspots are now cropping up. Take Germany, which quickly and efficiently battled the virus and has had one of the lowest death rates among the large northern European countries. Here, the R number – reflecting the average transmission rate – has risen again, below 1 until June 18, but rocketing to 2.88 just days later, only to drop again a few days later. It may be tempting to argue that this could be because the hotspots never got close to the 20% infection that was seen in other regions. But there are counter examples, albeit particularly in older and immunocompromised populations. In the Italian COVID-19 epicenter in Bergamo, a town where one in four residents are pensioners, 60% of the population had antibodies by early June. 
The same is true in some prisons: at the Trousdale Turner Correctional Center in Hartsville, US, 54% of inmates had tested positive for COVID-19 by early May. And more than half of the residents in some long-term care facilities have also been infected. Genes and environmentSo how do we explain this? Could people in places with higher rates of positive antibodies have a different genetic make-up? Early in the pandemic, there was much speculation about whether specific genetic receptors affected susceptibility to the SARS-CoV-2 virus. Geneticists thought that DNA variation in the ACE2 and TMPRSS2 genes might affect susceptibility to, and severity of, infection. But studies so far have shown no compelling evidence supporting this hypothesis. Early reports from China also suggested that blood types may play a role, with blood type A raising risk. This was recently confirmed in studies of Spanish and Italian patients, which also discovered a new genetic risk marker termed “3p21.31”. While genetics may be important, the environment also matters. It is well known that airborne transmission of droplets is enhanced in colder climates. Super-spreading events in several meat production facilities where the indoor climate is cold suggest this has enhanced contagion. People also tend to spend more time indoors and in close proximity during inclement weather. Warm weather, however, brings people together, albeit outdoors. Indeed, June has been uncharacteristically hot and sunny in many northern European countries, causing parks and beaches to be overrun and social distancing rules flouted. This will likely drive contagion and cause new COVID-19 outbreaks in the weeks to come. Yet another factor is how interpersonal interactions affect contagion. Some previous models have assumed that people interact in the same way regardless of age, well-being, social status and so forth. But this isn’t likely to be the case – young people, for example, are likely to have more acquaintances than the elderly. Accounting for this reduces the herd immunity threshold to around 40%. Will COVID-19 disappear?The lockdowns enforced far and wide, combined with the responsible actions of many citizens, have undoubtedly mitigated the spread of SARS-CoV-2 and saved lives. Indeed, in cases such as Sweden – where lockdown was eschewed and social distancing rules were relatively relaxed – the virus has claimed an order of magnitude more lives than in its pro-lockdown neighbours, Norway and Finland. But it is unlikely that lockdowns alone can explain the fact that infections have fallen in many regions after 20% of a population has been infected – something that, after all, happened in Stockholm and on cruise ships. That said, the fact that more than 20% of people have been infected in other places means that the T-cell hypothesis is unlikely to be the sole explanation either. Indeed, if a 20% threshold does exist, it applies to only some communities, depending on interactions between many genetic, immunological, behavioural and environmental factors, as well as the prevalence of pre-existing diseases. Understanding these complex interactions is going to be necessary if one is to meaningfully estimate when SARS-CoV-2 will burn itself out. Ascribing any apparent public health successes or failures to a single factor is appealing – but it is unlikely to provide sufficient insight into how COVID-19, or whatever comes next, can be defeated. Paul W Franks, Professor of Genetic Epidemiology, Lund University and Joacim Rocklöv, Professor of Epidemiology, Umeå University This article is republished from The Conversation under a Creative Commons license. Read the original article.
APOLOGIES TO MY ENGLISH READERS:
THIS BLOG AND EMBEDDED VIDEO IS ENTIRELY IN GERMAN
Inhaltsübersicht und Quellen:
bitte beachten - die jeweiligen Nummern zeigen die Abschnitte in diesem Video an, sind jedoch nicht auf das eingebettete Video koordiniert, sondern öffnen das Video in einem neuen Fenster an der gewählten Stelle.
Einige Quellenhinweise sind an CIDM.online gerichtet
▼
gratuitous click-bait - it just takes you to my home page.
Don't forget, I am first and foremost a artist. Please be advised that I am no longer associated with Printful. I deleted the Store App for it and closed my account there. Disregard any pop-up advertisement on my website for any items offered through Printful. The "shopping cart" that appears on top of my website is an error that hopefully goes away, since I do not have an integrated web shop on here anymore! I HAVE PRINT SERVICES AND MERCHANDISE WEBSITES SET UP AT OTHER SITES, THE LINKS TO WHICH YOU FIND ON EVERY PAGE ON THE FOOTER. You could also consult my LINKS page. Additionally, on every artwork page there are links where prints of my art are available.
MORE QUESTIONS & A FEW ANSWERS
Firstly, allow me a bit of self-promotion - we get to the serious questions after this:
As I am doing research, I am asking questions to which I do not always receive adequate answers.
So I keep digging. Here are some ABSTRACTS from which I hope to build my case:
FROM CONVERSATIONS I HAD ON WHATSAPP AND FACEBOOK:
(translate to English and show side by side with German)
WhatsApp:
Angst vor CoV bremst Öffi-Verkehr
(▲ article in German)
Facebook:
The latest news from Prof. Hendrik Streeck and the Heinsberg Study
published June 7th 2020 in RP-ONLINE article is in German, use Google Translate: Bonner Virologe Streeck plädiert für „mehr Mut“ im Sommer Bonn virologist Streeck pleads for "more courage" in summer
PROMISING LINKS
I am quoting short excerpts from these articles please click the links to read more:
ASYMPTOMATIC SPREAD MAKES TESTING KEY FOR COVID-19 FIGHT
MAY 15TH, 2020 POSTED BY JOHNS HOPKINS UNIVERSITY
The prevalence of asymptomatic cases—people infected with the virus who can spread it to others but don’t feel sick—is one of the most challenging aspects of the coronavirus pandemic, researchers say.
Current testing methods can detect asymptomatic cases. When you are infected with the coronavirus, the tests are pretty sensitive to any presence of the virus. The most common test at the moment is a PCR test, which looks for the presence of the virus’s genetic material, and some of these are more sensitive than others.
What it means to be immune to the coronavirus
April 14th 2020 in MASHABLE
"The golden rule of immunology is if you are infected with a virus, get sick, and recover, you probably won't get reinfected with the same virus," said Mark Cameron, an immunologist at Case Western Reserve University who previously helped contain the outbreak of another deadly coronavirus, SARS, in 2003.
Why, though, might a significant number of people have such mild (or no) symptoms to this new coronavirus? There could be genetic or health differences that make it more difficult for the coronaviruses to infect a cell. It's also possible that people with milder infections were only exposed to a tiny amount of the virus (like someone picking up just a few particles off a piece of mail versus an ER doctor getting sprayed with millions of viral particles). "It's possible that asymptomatic people were exposed to a much lower dose," said Brian Baker, a biochemist at the University of Notre Dame.
At the end of the day, this coronavirus may unwittingly help humanity tame the pandemic. While it's true that asymptomatic people can spread the virus when they're infected (that's why everyone must social distance right now), if one in four infected people are truly asymptomatic, that means that likely millions of people will ultimately develop immunity — whether they know it or not — and won't be able to spread the virus around until we get a vaccine. "That would be a good thing," said Baker.
"We can count on the fact that the vast majority of COVID infections will cause immunity," said Cameron, noting that a vaccine will then only add to the number of immune people. Ultimately, this is how we end this grim pandemic, now that we've failed to contain it.
|
OTTO RAPPThis blog is primarily art related - for my photography please go to Archives
April 2024
Categories
All
|





 RSS Feed
RSS Feed