|
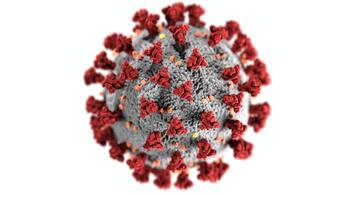
The news about anything to do with Corona is overwhelming - if one is on Twitter and Facebook alone it is already too much, add to that all the messages on Messenger, WhatsApp and other channels can make ones head explode.
Lately, I tried to make sense out of some of this, and somehow, a pattern emerged by putting it all in order.
I published a long blog on the Hive Blockchain, and I won't just copy it all over on this one,
but simply link to it (it is publicly available everywhere):
▲
click for the whole story
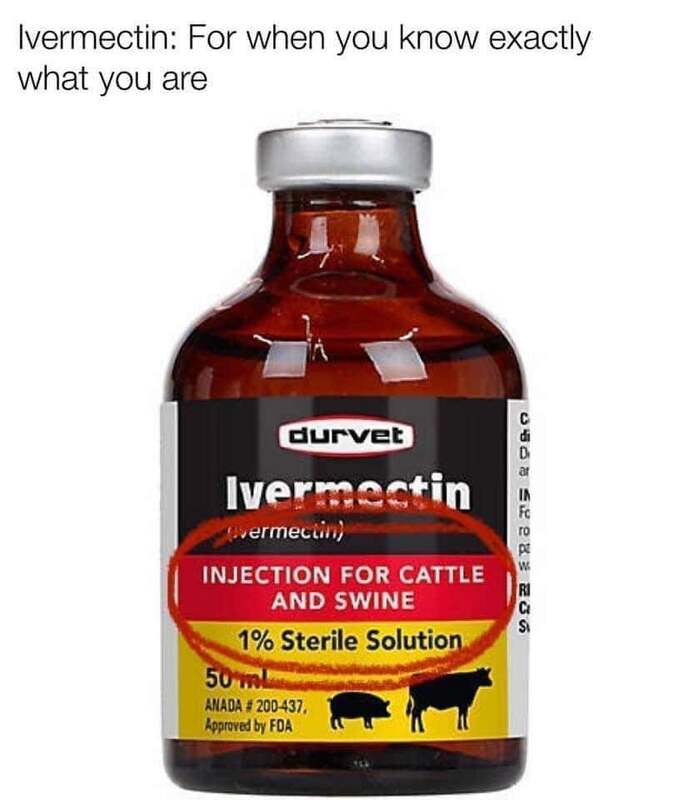
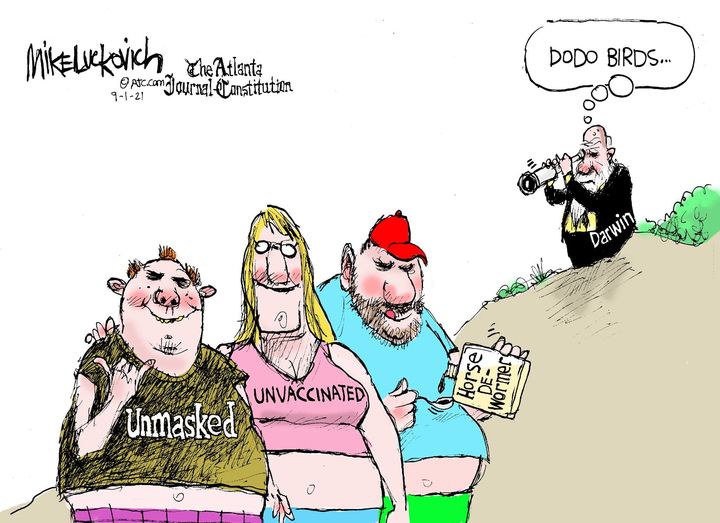
Just for the fun of it, I include some insane memes I found on Facebook, which are not part of the Hive blog. If anyone feel 'outed' or embarrassed about it, they should not have posted them.
A search on Facebook on thetopic of Corona would keep one occupied until the end of times. Some serious, some funny, but most of it insanely dumb, particularly the comments.
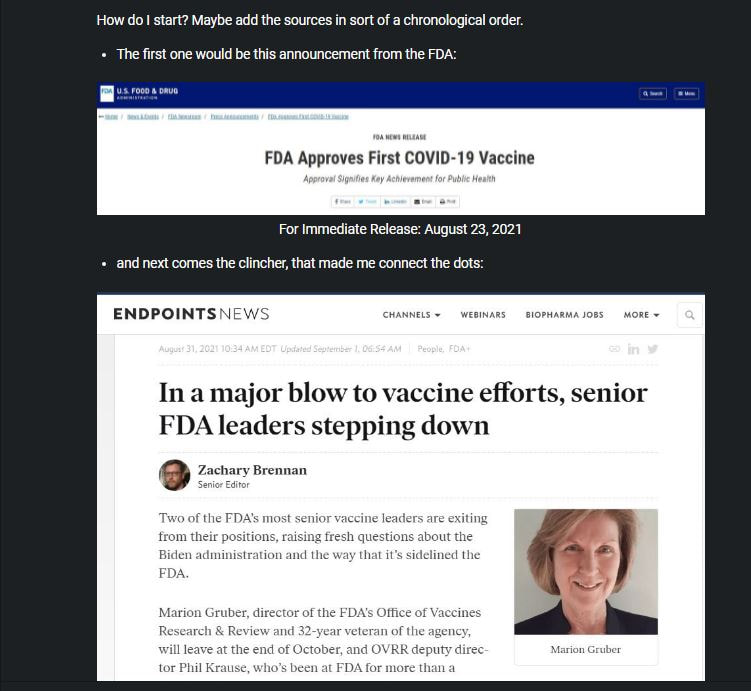
I have been gathering a number of resources about these vaccines that are currently on the market. I am rather cautious and not given to conspiracy theories, so I select my resources carefully. What concerns me at this time is that adverse reactions to these vaccines, all of which are only under a temporary emergency use authorization, are alarmingly mounting, but news about it had been being suppressed.
But more of it is being reported now, and not just by "conspiracy theorists", but reputable news and government sources, it can no longer be ignored. I present a selection of items which I shared on Twitter. But first, for the sake of being thorough and fair, here is a video by the FDA explaining the Drug Approval Process:
The process is similar in Europe and other places in the world. Check out how the WHO explains it:
WHO lists additional COVID-19 vaccine for emergency use and issues interim policy recommendations
A interesting read would be this, and perhaps read it first before continuing here - the link opens in a separate window:
What does full FDA approval of a vaccine do if it’s already authorized for emergency use?
Apropos FDA, you might want to check out and follow the link on this tweet:
— Otto Rapp (@ArtOfTheMystic) August 13, 2021 here are some select tweets i posted or shared lately:— Otto Rapp (@ArtOfTheMystic) August 20, 2021
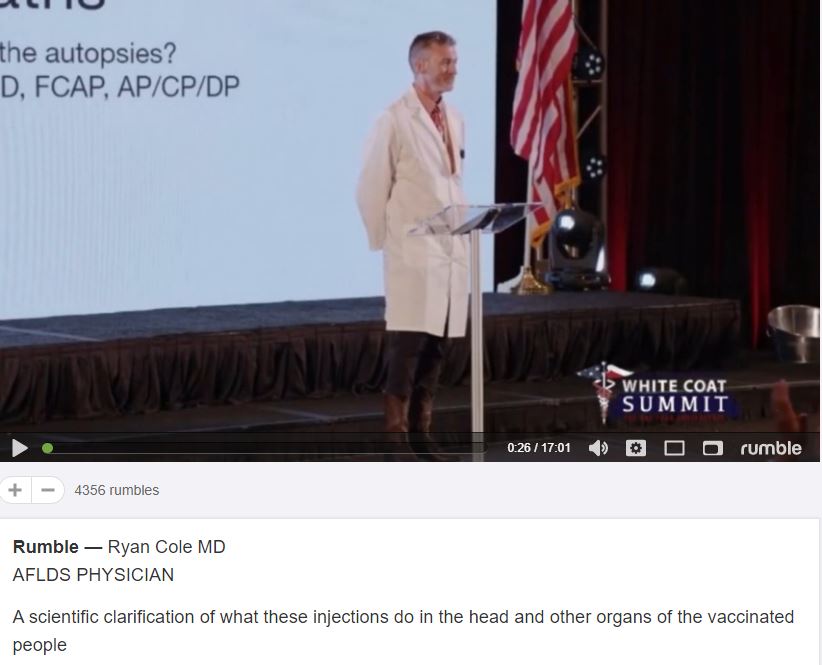
Now I like to present something that some may consider controversial - videos such as these are often banned on social media sites and YouTube. A shame really, because a exchange of ideas is often impossible and only one side, the officially sanctioned opinion, is presented. But like I mentioned above, more of it is also appearing now in the main stream media.
A PATHOLOGIST SUMMARY OF WHAT THESE JABS DO TO
|
|
ENGLISH Comments
Talk about 100,000 dead first, then wonder that people are scared and afraid!
A political failure at all levels! How does it look like: Austrian Ministry of Health Dashboard So at this time 437 people are currently sick in all of Austria! Statistically speaking, what are the chances that you will encounter one of them (who should be in quarantine) on the public transport in Vienna, and he will then also cough on us! Quote from the text: "In order to reverse the trend again, the company is trying to reduce the fear of infection among passengers. On the one hand, reference is made to the study by AGES (Agency for Health and Food Security) presented on May 6 that no cluster infections had been reported so far - meaning no occurrence of frequent cases in public transportation." |
DEUTSCHE Kommentare
Zuerst über 100.000 Tote reden, dann wundern sie sich das die Menschen verschreckt sind und sich fürchten!
Ein politisches Versagen auf allen Ebenen! Wie sieht es aus: Österreichisches Gesundheitsministerium Dashboard Also momentan 437 Aktuell Erkrankte in ganz Österreich! Statistisch gesehen, was sind die Chancen dass man einen davon (der sich ja in Quarantäne befinden sollte) auf den Öffis in Wien begegnet der uns dann auch noch anhustet! Zitat von dem Text: "Um den Trend wieder umzukehren, bemüht sich das Unternehmen, die Angst vor einer Ansteckung bei den Fahrgästen zu nehmen. Einerseits verweist man auf die am 6. Mai präsentierte Studie der AGES (Agentur für Gesundheit und Ernährungssicherheit), wonach bisher kein einziger Infektions-Cluster – also das Auftreten gehäufter Fälle – in Öffis aufgetreten sei." |
|
The restrictions don't stop until there is a vaccine or an effective drug. I really don't want to be vaccinated with the Gates miracle syringe. An effective drug? it never existed against corona viruses, there will never be. Tamiflu against a flu that was barely noticeable. And vaccine against swine flu where people got really sick afterwards. Now they want to play around with RNA, intervene in our DNA - this can have bad consequences because the test subjects would first have to be observed for years whether they might not get cancer. We are upset about genetic engineering in our food, so do we want to inject genetic engineering into people? This week in the Zeit (magazine): The vaccine inventors from BioNTech. Links below are all in German: Im Team gegen Corona My Research: Erste Teilnehmer von Biontech-Studie in den USA geimpft Quote: "In search of a vaccine against SARS-CoV-2, the first tests by the Mainz-based company Biontech and the US company Pfizer have also started in the United States. The companies said that the first subjects had been treated. The candidate vaccine is an experimental RNA vaccine." They have been on the radar since April. Successful with stock market price through press releases. Much like the gold exploration companies - are always on the lookout. Now and then promising reports. And then: Bre-X Quote from Wer ist Biontech? "The share price is, at least for many investors, the measure of a company's success. In the middle of the week, that of the Mainz-based biotechnology group Biontech on the US technology exchange Nasdaq rose to almost $ 56. That was an increase of more than 30 percent in a single day." I am interested in the so-called dark figures. We have to wear masks because we could possibly be asymptomatic virus throwers. But my question: should I have caught the virus, be asymptomatic, then after some time my immune system should have successfully fought the virus - as well as every other sick person who has then recovered. Thus, like the recovered, I am part of herd immunity. That would also explain why the number of cases did not go up despite loosening, meetings, demos, hardware stores, Easter, Pentecost, etc. I've had a lot of experience with corona virus. The last time I was sick in 2012 was when I was hit hard. Nothing since then, and hardly ever before. |
Die Beschränkungen hören erst gänzlich auf, wenn es einen Impfstoff oder ein wirksames Medikament gibt.
Mit dem Gates seiner Wunderspritze lass ich mich aber wirklich nicht impfen. Ein wirksames Medikament? gab es niemals gegen Coronaviren, wird es auch nie geben. Tamiflu gegen eine Grippe die kaum bemerkbar war. Und Impfstoff gegen die Schweinegrippe wo Menschen daraufhin erst so recht krank wurden. Jetzt wollen sie mit RNA herumspielen, in unser DNA eingreifen - das kann schlechte Folgen haben denn die müssten Probanden erstmal jahrelang beobachten ob die nicht vielleicht Krebs davon bekommen. Wir regen uns über Gentech in unserer Nahrung auf, und da wollen sie Gentech in Menschen einspritzen? Diese Woche in der Zeit: Die Impfstoff-Erfinder von BioNTech. Link: Im Team gegen Corona Mein Research: Erste Teilnehmer von Biontech-Studie in den USA geimpft Zitat: "Auf der Suche nach einem Impfstoff gegen SARS-CoV-2 sind mittlerweile auch die ersten Tests des Mainzer Unternehmens Biontech und des US-Unternehmens Pfizer in den Vereinigten Staaten angelaufen. Die erste Probanden seien behandelt worden, teilten die Firmen nun mit. Es handelt sich bei der Kandidatvakzine um einen experimentellen RNA-Impfstoff." Die sind schon seit April am Radar. Mit Börsenkurs durch Presseaussendungen erfolgreich. Ungefähr so wie die Goldexploration Firmen - sind immer auf der Suche. Ab und zu vielversprechende Meldungen. Und dann: Bre-X Quote von Wer ist Biontech? "Der Aktienkurs ist zumindest für viele Investoren das Maß für den Erfolg eines Unternehmens. Mitte der Woche ging der des Mainzer Biotechnologiekonzerns Biontech an der US-Technologiebörse Nasdaq bis auf fast 56 Dollar in die Höhe. Das waren ein Plus von mehr als 30 Prozent an einem einzige Tag." Mich interessieren die sogenannten Dunkelziffern. Wir müssen ja Masken tragen weil wir möglicherweise asymptomatische Virenschleudern sein könnten. Meine Frage aber: sollte ich das Virus erwischt haben, asymptomatisch sein, dann müsste ja nach einiger Zeit mein Immunsystem das Virus erfolgreich bekämpft haben - sowie auch bei jedem anderen Erkrankten der dann genesen ist. Somit bin ich, eben so wie die Genesenen, ein Teil der Herdenimmunität. Das würde auch erklären warum die Fallzahlen trotz Lockerungen, Versammlungen, Demos, Baumarkt, Ostern, Pfingsten usw nicht in die Höhe gegangen sind. Ich habe so einiges erlebt in Bezug auf Corona Viren. Letztes Mal war ich in 2012 krank, da hat es mich gut erwischt. Seither nichts mehr, und kaum je vorher. |
published June 7th 2020 in RP-ONLINE
article is in German, use Google Translate:
Bonner Virologe Streeck plädiert für „mehr Mut“ im Sommer
Bonn virologist Streeck pleads for "more courage" in summer
|
Quote: "Virologist Hendrik Streeck sees an opportunity to fight the corona pandemic during the summer months. Partial immunity could possibly be built up in the population."
|
Zitat: "Bei der Bekämpfung der Corona-Pandemie sieht der Virologe Hendrik Streeck eine Chance während der Sommermonate. Es könne möglicherweise eine Teilimmunität in der Bevölkerung aufgebaut werden."
|
I am quoting short excerpts from these articles
please click the links to read more:
MAY 15TH, 2020
POSTED BY JOHNS HOPKINS UNIVERSITY
April 14th 2020 in MASHABLE
Genetic vaccines against COVID-19: hope or RISK?
The video was originally uploaded in German on May 3rd, he has now dubbed it in English and posted on May 10th. Thus, this important information is available to a much wider audience.
english |
deutsch |
For best viewing, go to full screen.
We must urgently develop measures to tackle the new coronavirus
— but safety always comes first, says Shibo Jiang.
and at the New York Blood Center, New York, USA.
Around the world, I am seeing efforts to support ‘quick-fix’ programmes aimed at developing vaccines and therapeutics against COVID-19. Groups in the United States and China are already planning to test vaccines in healthy human volunteers. Make no mistake, it’s essential that we work as hard and fast as possible to develop drugs and vaccines that are widely available across the world. But it is important not to cut corners.
Vaccines for measles, mumps, rubella, polio, smallpox and influenza have a long history of safe use and were developed in line with requirements of regulatory agencies.
I have worked to develop vaccines and treatments for coronaviruses since 2003, when the severe acute respiratory syndrome (SARS) outbreak happened. In my view, standard protocols are essential for safeguarding health. Before allowing use of a COVID-19 vaccine in humans, regulators should evaluate safety with a range of virus strains and in more than one animal model. They should also demand strong preclinical evidence that the experimental vaccines prevent infection, even though that will probably mean waiting weeks or even months for the models to become available.
Journal Human Vaccines Volume 2, 2006 - Issue 2
DNA vaccines are based on the transfer of genetic material, encoding an antigen, to the cells of the vaccine recipient. Despite high expectations of DNA vaccines as a result of promising preclinical data their clinical utility remains unproven. However, much data is gathered in preclinical and clinical studies about the safety of DNA vaccines. Here we review current knowledge about the safety of DNA vaccines. Safety concerns of DNA vaccines relate to genetic, immunologic, toxic, and environmental effects. In this review we provide an overview of findings related to the safety of DNA vaccines, obtained so far. We conclude that the potential risks of DNA vaccines are minimal. However, their safety issues may differ case-by-case, and they should be treated accordingly.
There were discussions on Facebook about the subject of vaccines, lock-downs and possible second and third waves of COVID-19. I just want to pick out one, followed by my answer.
What do you know about SARS? Where is it now, how many "waves" of it since 2003 - just for an example. Pandemics such as these run their course in due time. By the time they have a vaccine (if ever - i.e. there never was one found for SARS*) it will have run its course and the vaccine irrelevant to go on the trash heap - but if it mutates, then the vaccines will be useless anyway, the same as many of the flu vaccines were useless, and some, like the swine flu, were even dangerous. But Pharma will have made billions in profit.
The way it is going now (with exceptions of a few bad pockets that are cited as scare stories) the curves are flattening, so in order to keep up the pharma propaganda, there has to be the specter of new waves projected, and as some say, much worse than the original - because without fear (which by itself lowers your immune system) they cannot exert the type of desired control to turn people into obedient robots.
Lets just drink the Cool-Aid.
So any claim that we can never return to normal unless there is a vaccine and everyone is vaccinated, is
irresponsible scaremongering. The fact hat such comes from the chancellor of Austria is however alarming.
To speculate what is behind all this, I leave to others - and you, dear reader: what does your common sense tell you?
As of 2020, there is no cure or protective vaccine for SARS that has been shown to be both safe and effective in humans. According to research papers published in 2005 and 2006, the identification and development of novel vaccines and medicines to treat SARS was a priority for governments and public health agencies around the world. In early 2004, an early clinical trial on volunteers was planned. A major researcher´s 2016 request, however, demonstrated that no field-ready SARS vaccine had been completed because likely market-driven priorities had ended funding. ............ Wikipedia - SARS Treatment
well, yeah, but it is a strain of SARS
so what about SARS?
April 2006
By 2004, SARS cases had slowed just as mysteriously as they had started in Guandong province of southern China 2 years earlier, in December of 2002. Yet the legacy of unanswered questions the pathogen left behind should keep scientists, public health officials, epidemiologists, and ethicists occupied for a long time to come. Why, exactly, should we revive discussion if it is no longer a pressing threat? After all, the SARS death toll is relatively low with 812 deaths worldwide. What’s more, the looming H5N1 avian flu virus is currently front page news. Even so, the SARS epidemic should not be filed away without appreciation of the lessons it taught.
Although short-lived, SARS forced us to face the unpleasant reality of global pandemics and to address the ethico-legal dilemmas that result from hasty public health measures.
Don't forget, I am first and foremost a artist.
OTTO RAPP
This blog is primarily art related - for my photography please go to
Otto Rapp Photo Blog
*
Since April 2020 I have also dedicated a category of my blog to the current Corona Virus crisis.
Archives
April 2024
January 2024
November 2023
October 2023
March 2023
January 2023
June 2022
May 2022
April 2022
March 2022
January 2022
December 2021
November 2021
October 2021
September 2021
August 2021
July 2021
June 2021
May 2021
April 2021
March 2021
February 2021
January 2021
November 2020
October 2020
September 2020
August 2020
July 2020
June 2020
May 2020
April 2020
March 2020
February 2020
December 2019
November 2019
September 2019
May 2019
April 2019
March 2019
November 2018
October 2018
September 2018
July 2018
February 2018
January 2018
September 2017
August 2017
July 2017
May 2017
April 2017
March 2017
February 2017
January 2017
November 2016
October 2016
September 2016
June 2016
May 2016
April 2016
March 2016
February 2016
January 2016
December 2015
November 2015
October 2015
September 2015
August 2015
July 2015
June 2015
May 2015
April 2015
March 2015
February 2015
December 2014
November 2014
October 2014
September 2014
August 2014
July 2014
May 2014
April 2014
February 2014
January 2014
December 2013
November 2013
October 2013
September 2013
March 2013
February 2013
Categories
All
123RF
3D Printing
A CHANCE FOR HAPPINESS
Alberta
Animal Farm
Animation
Archaic Visions
Art Basel
Art Criticism
Art Fair
Art Gallery
Art History
Artisteem
Artists
Art Of The Mystic
Art Of Where
Atelier Modovan
Australia
Austria
Biennale
Biology
Birthday
Blockchain
Blogs
Blurb
Book
Bruce Rimell
Cafe Kosmos
Calendar
Calgary
Canada
Caroline Schell
Castle Gloggnitz
Catalog
Censorship
Ceramics
CHARITY
Chimeria
Christmas
Civil Disobedience
Clemens Arvay
Clothing
Conceptual Art
Conspiracy Theories
Contest
Corinna Herden
Corona Virus
Crazy
Cult
Deep Dream
De Es Schwertberger
Defamation
Demons
Demonstration
Designs
Digital Art
Documentary
Domestic Abuse
Drawing
Drawings
Dreams & Divitities
Emily Levy
Ernst Fuchs
Ernst Fuchs Museum
Exhibition
Facebook
Face Masks
Family
Fantastic Art
Fantastic Art Shop
Fantastic Realism
Fantastic Realism
Fantasy
Fashion
Fine Art
Fine Art America
Flickr
Friends
Fritz Janschka
Fundraising
Gallery Bator
Garden Of Fernal Delights
George Orwell
Gesichtsschutz
GIF Generator
Graduation
Grand Salon 2017
Grand Salon 2018
Greece
Group Show
Harlan Ellison
Heinsberg Study
Henry David Thoreau
Hieronymus Bosch
Holiday
Humor
Immune System
Infeld
Instagram
International Surrealism Now
Internet
Isabella Bogner Bader
Isolation
Ivermectin
Jason Rapp
Jos Pirkner
Kunstquartier Wien
LAXENBURG
Leisure
Liba W Stambollion
Magical Dreams
Magic Realism
Medicines
Memorial
Mental Health
Merchandise
Met Museum
Minerva Art Gallery
Modern Art
Movie
Music
Mythology
Nature
Nautilus Studio
Neuroscience
News
Obituary
Omicron
One Art Space
Open House
Open Studio
Otto Rapp
Otto Rapp
Painting
Paintings
Performance Art
Phantastik In Der Box
Photobucket
Photography
Pigmalion
Pinterest
Pixels
POD
Poetry
Pollution
Portrait
Portugal
Poster Art
Post-modernism
Prints
Prof. Dr. Hendrik Streeck
Promotion
Psychology
Public Collections
Quantum Theory
Religion
Reminiscing
Research
Rosenmaedchen
Rue Morgue Magazin
Sale
Satire
Science
Sculpture
Serbia
Shahram Alizadeh
Shoes
Social Isolation
Social Networks
Society For Art Of Imagination
Soundcloud
Steem
Steemit
Surrealism
Theater
The Conversation
The Painted Word
Tom Wolfe
T-shirts
Ukraine
University Of Lethbridge
Vaccines
Video
Viechtach
Vienna
Vienna Academy Of Visionary Art
Vienna School Of Fantastic Realism
Villa Berberich
Visionary
Visionary Art
Vocativ
Website
Weebly
WINGNUTS
Woodstock
Workshop
Writing
Yvette Endrijautzki
Zazzle








 RSS Feed
RSS Feed