|
2020 / 2022 - For the past two years, the world population has been under the spell of the coronavirus. Emergency regimes have been established, civil liberties have been dismantled, surveillance programs were being installed and an unprecedented global vaccination program has been rolled out.
Are we doing the right thing, or did we make a deal with the devil in exchange for a benefit? Through critical voices from various areas of expertise, PANDAMNED attempted for the first time to paint the whole picture and shed light on the darkness. It has become a relentless stocktaking of our time, which global organizations, governments and big tech companies would have preferred to prevent. Documentary maker Marijn Poels takes the viewer on an enlightening journey through the emerging absurd world of the "New Normal" and how we can still prevent it. www.pandamned.org Subtitles: German, Englisch, Dutch For my German readers, here is a excellent article in German für meine Deutschen Leser, hier ist ein sehr guter Artikel auf Deutsch über diesen Film: «Pandamned» – Dokumentation über die Hintergründe der Corona-Politik
After getting messages about this I decided to one more time add something about it in my blog.
Bloomberg SurveillanceTV Shows
January 5th, 2022, 1:19 PM GMT+0100 Johns Hopkins University Associate Professor of Emergency Medicine Bhakti Hansoti discusses confusion over Covid messaging, issues around access to testing, and the differences between rapid and PCR tests. The Bloomberg School of Public Health is supported by Michael R. Bloomberg, founder and majority owner of Bloomberg LP, the parent company of Bloomberg News. (Source: AFP)
January 10th, 2022, 1:46 PM GMT+0100
Johns Hopkins Bloomberg School of Public Health Vice Dean Joshua Sharfstein discusses how the Covid-19 pandemic may look after the omicron wave and antibody protection from a coronavirus infection. The Bloomberg School of Public Health is supported by Michael R. Bloomberg, founder and majority owner of Bloomberg LP, the parent company of Bloomberg News. (Source: AFP)
A article from January 11th is also interesting, in respect to vaccinations and the call for mandatory vaccines:
European Union regulators warned that frequent Covid-19 booster shots could adversely affect the immune response and may not be feasible.
Repeat booster doses every four months could eventually weaken the immune response and tire out people, according to the European Medicines Agency. Instead, countries should leave more time between booster programs and tie them to the onset of the cold season in each hemisphere, following the blueprint set out by influenza vaccination strategies, the agency said.
Das habe ich zuerst mal auf Facebook gesehen, dann das Original auf Bitchute gefunden. Die obige Illustration ist ein Holzschnitt aus einer Ausgabe von Das Narrenschiff aus dem 15th Jahrhundert. Bis Heute hat sich meiner Ansicht nach nicht viel geändert.
Dieses Video ist für Menschen gemacht, die bei der "Pandemie" lange mitgemacht haben, denen aber mittlerweile das eine oder andere schon etwas seltsam vorkommt. Ideal also, um es an Freunde und Bekannte weiterzuleiten, die Euch bislang für Spinner oder Verschwörungstheoretiker gehalten haben, bei denen aber noch Hoffnung besteht. Widersprüche in der offiziellen Lesart der "Pandemie" gibt es auch in den normalen Massenmedien, man muss nur danach suchen. Ich habe Dutzende Ausschnitte von Zeitungen zusammengeschnitten, die zeigen, dass sich die wenigen von Politik und Medien akzeptierten und hofierten auserwählten "Fachleute" alle paar Wochen selbst widersprechen. Ich zeige auch, dass es sehr wohl in den "seriösen und anerkannten" Medien hier und da eine kritische Stimme gibt, die die Wahrheit klar benennt. Diese Stimmen werden nur meist von Lauterbachs Panikgeschwafel und Drostens apokalyptischen Phantasien niedergebrüllt. MichaelLeitner This video was sent to me via WhatsApp. This is the Live-stream from the demo today: Today is the time. Austria goes on the street together for FREEDOM! Today Vienna sets a sign against the newest Lockdown insanity and forced vaccinations! :Yesterday I posted on the Blockchain - embedded on Twitter - please click through to the original post, there is a lot of information, relevant videos and newspaper articles.
I could not help myself - here is my interpretation of the mayor of Vienna one of the driving forces of the measures against which the people are protesting UPDATE November 21st 2021 posted on the blockchain with additional material and details:
Short and sweet today - below find embedded a chart from ourworldindata.org where I selected a number of countries to compare. Mouse over the timeline and observe the changing rankings.
I included India for various reasons, one being that the Delta variation had originally been called the Indian variation, the other is that even though the vaccination rate in India is around 10%, it has now for the longest time one of the lowest fall numbers in the world.
Included in this chart is Austria, where I live. What I think about the current "Measures" I point out here (which I also published on Facebook):
The policies in force now in Austria are pure insanity!
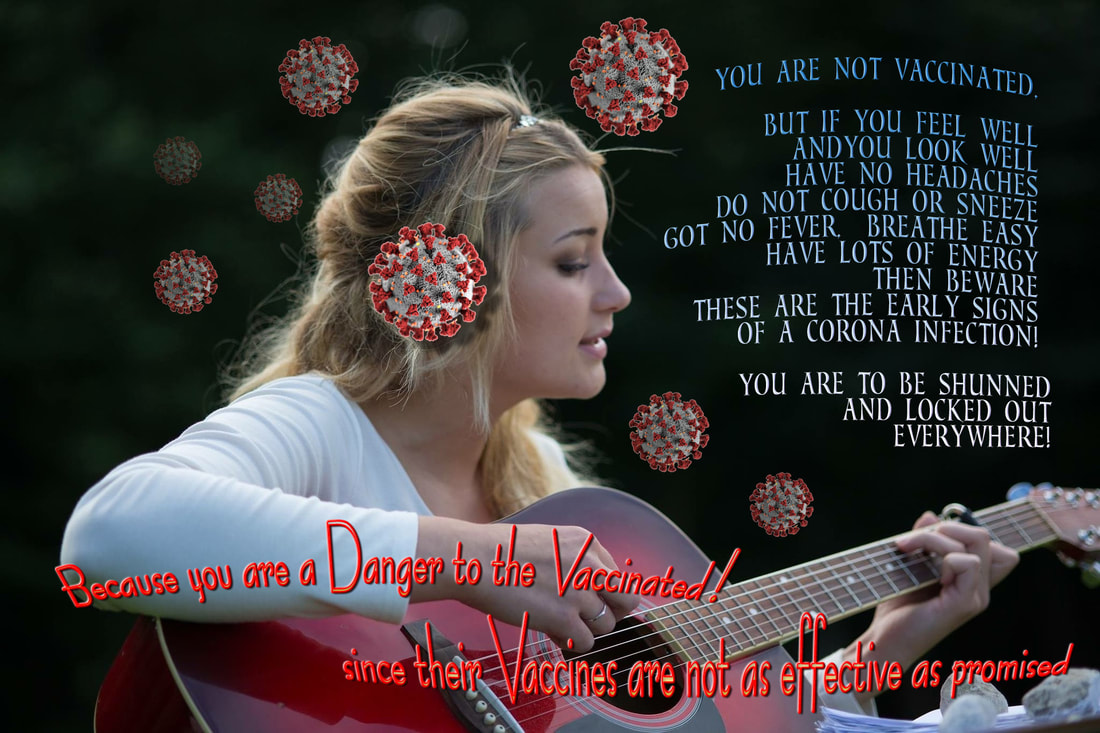
There is a campaign going on to blame the unvaccinated for everything. But it will soon show the truth, because now the unvaccinated are in lockdown, whereas the vaccinated are free to do everything and are not required to be tested. Considering the decreasing efficiency of the vaccines, that one can be infected and infectious, we should see (and already have) where the cluster infections will happen, and how many vaccinated are filling the hospitals (the percentages are rising - at the moment it is 40% vaccinated). The vaccinated were from the start given to believe that the vaccines are highly effective, and from the comments in the media we can see that the majority believe that now they are free to do whatever, no precautions, no masks, party without care. The ones that are actually careful and mindful of the virus are those that are unvaccinated (and a few of the vaccinated that have enough brains) which are wearing masks, hold proper distance and follow all hygiene recommendations. In my circles I know quite a few vaccinated people that did catch the virus, and some quite bad, whereas I am not aware that any of my unvaccinated friends are sick - even though one particularly disturbed so called "Virologist", Dorothee von Laer, proclaimed that 3G (as a rule is called in German) actually means Geimpft - Genesen - Gestorben (translated: Vaccinated - Recovered - Dead) - the third G actually means Getestet = tested. And this are the so called experts that advise the government of Austria. If you read German, or have a translator installed, check this out, it is unreal, and I commented previousl on Facebook that she should be a prime candidate for psychiatric attention: https://www.weekend.at/politik/virologin-von-laer-duestere-3G-prognose
This also as a comment on the current video about the subject by Dr. John Campbell:
Bonus today - a very interesting video that brings together eight prominent medical experts, among themDr. Robert W. Malone who was instrumental in the development of mRNA vaccine.
I REALIZED I HAD NOT POSTED LATELY UNDER THE TAG CORONA - I HAD HOWEVER CONTRIBUTED A FEW RELEVANT POSTS ON FACEBOOK AND MY BLOCKCHAIN ACCOUNT.
So here we go - I posted the most important blogs just now on the Hive/PeakD blockchain. So rather than preaching twice, I just give you the highlights here.
Visions of Corona - the pandemic has the city in its grip.
Digital photocollage. Coronavirus - Aktuelle Maßnahmen in Österreich CORONA WAHNSINN - CORONA MADNESS
click text link above to see the entire article - opens in separate window - most content is in German
but some items are also in English, and one particularly relevant text had been translated. Among the items of interest is how Denmark handles Corona, so below find embedded the current DANISH CORONA PASS
▲
Es ist unerklärlich warum das bei uns nicht funktionieren könnte It is inexplicable why this could not work for us to read up on the Danish site, go to coronasmitte.dk After posting on the Blockchain, I found this video about a protest in Vienna (in German):
I also like to point out that some of the most interesting posts are collected on my Mix site under the Covid-19 Collection:
Also contained in my Blockchain Blog CORONA WAHNSINN - CORONA MADNESS is the interesting story of the Irish City District Waterford where it says that:
Waterford city has one of the Ireland’s highest rates of vaccination against Covid-19, but one of its electoral areas has emerged as the place with the highest rate of Covid-19 infection in the State.
The news about anything to do with Corona is overwhelming - if one is on Twitter and Facebook alone it is already too much, add to that all the messages on Messenger, WhatsApp and other channels can make ones head explode.
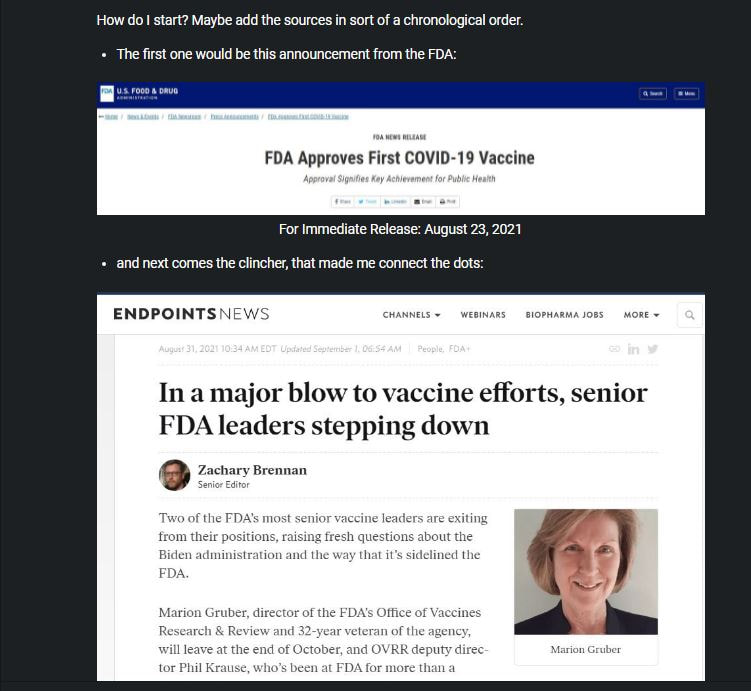
Lately, I tried to make sense out of some of this, and somehow, a pattern emerged by putting it all in order.
I published a long blog on the Hive Blockchain, and I won't just copy it all over on this one,
but simply link to it (it is publicly available everywhere):
▲
click for the whole story
Just for the fun of it, I include some insane memes I found on Facebook, which are not part of the Hive blog. If anyone feel 'outed' or embarrassed about it, they should not have posted them.
A search on Facebook on thetopic of Corona would keep one occupied until the end of times. Some serious, some funny, but most of it insanely dumb, particularly the comments. 
First off, maybe check who David E. Martin, PhD is - lets visit the website of his company M.CAM: https://www.m-cam.com/about-us/ I am not going to write a long intro, because whatever I could say could not do justice of what is being discussed in these videos.
The first video I was made aware of by a Canadian friend, and it discussed issues about the Corona Virus from a Canadian perspective. It was uploaded to BitChute by Vaccine Choice Canada:
After watching this, I started searching and found the info about his company (see above), but additional videos, and one of them from the Stiftung Corona Ausschuss, conducted in Berlin, Germany, but all in English
This is a multiple-warhead bombshell: Intelligence analyst David E. Martin has been checking the patent files concerning SARS-CoV2 and found out ... damn, listen to the guy yourself. If this turns out to be true there can be no more doubt about what the hell is going on.
The German Corona Inquiry Committee has been formed in July 2020 and heard almost 150 scientists, experts, researchers, witnesses and victims in 60 five-hour sessions. This video is a collection of the English-only sections of the hearing. The hearing with David E. Martin can be watched completely at: Dr. David E. Martin | Sitzung 60: Die Zeit ist kein flacher Kreis
You might want to watch either of these two videos at the origin sites BitChute and YouTube, since some of the comments would also be interesting. The video on the Corona Ausschuss website is a little longer than the one on YouTube.
I have been gathering a number of resources about these vaccines that are currently on the market. I am rather cautious and not given to conspiracy theories, so I select my resources carefully. What concerns me at this time is that adverse reactions to these vaccines, all of which are only under a temporary emergency use authorization, are alarmingly mounting, but news about it had been being suppressed.
But more of it is being reported now, and not just by "conspiracy theorists", but reputable news and government sources, it can no longer be ignored. I present a selection of items which I shared on Twitter. But first, for the sake of being thorough and fair, here is a video by the FDA explaining the Drug Approval Process:
The process is similar in Europe and other places in the world. Check out how the WHO explains it:
WHO lists additional COVID-19 vaccine for emergency use and issues interim policy recommendations
A interesting read would be this, and perhaps read it first before continuing here - the link opens in a separate window:
What does full FDA approval of a vaccine do if it’s already authorized for emergency use?
Apropos FDA, you might want to check out and follow the link on this tweet:
— Otto Rapp (@ArtOfTheMystic) August 13, 2021 here are some select tweets i posted or shared lately:— Otto Rapp (@ArtOfTheMystic) August 20, 2021
Now I like to present something that some may consider controversial - videos such as these are often banned on social media sites and YouTube. A shame really, because a exchange of ideas is often impossible and only one side, the officially sanctioned opinion, is presented. But like I mentioned above, more of it is also appearing now in the main stream media.
A PATHOLOGIST SUMMARY OF WHAT THESE JABS DO TO
|
OTTO RAPPThis blog is primarily art related - for my photography please go to Archives
April 2024
Categories
All
|










 RSS Feed
RSS Feed