Ich finde es eher beängstigend, dass offenbar bei fast allen europäischen Politikern die Sicherungen durchknallen.Sehr prominent auf meinem X (Twitter) Feed. Geht es noch? Ist das eine Rückkehr auf Stasi Verleumdungen? Es wird noch ganz offen über ein Verbot der AfD gesprochen! Wer sind denn wirklich die 'Rechtsextremisten'? https://platform.twitter.com/widgets.js Eine der besten Antwortenhttps://platform.twitter.com/widgets.js Und das hier beantwortet wer eigentlich die Extremisten sindhttps://platform.twitter.com/widgets.js https://platform.twitter.com/widgets.js UM DAS GEHT ES HIERWenn etwas verboten werden sollte, dann sind es die Linksextremen Hetzportale und Volksverpetzer, wie eben auch solche links-finanzierte Schmutzkübel wie Correctiv.https://platform.twitter.com/widgets.js Nur so zur Erinnerung – ‘Das beste Deutschland aller Zeiten’????? https://blackout-news.de/aktuelles/wirtschaftlicher-absturz-wie-fehlentscheidungen-und-politik-in-deutschland-die-wirtschaft-bedrohen/ 
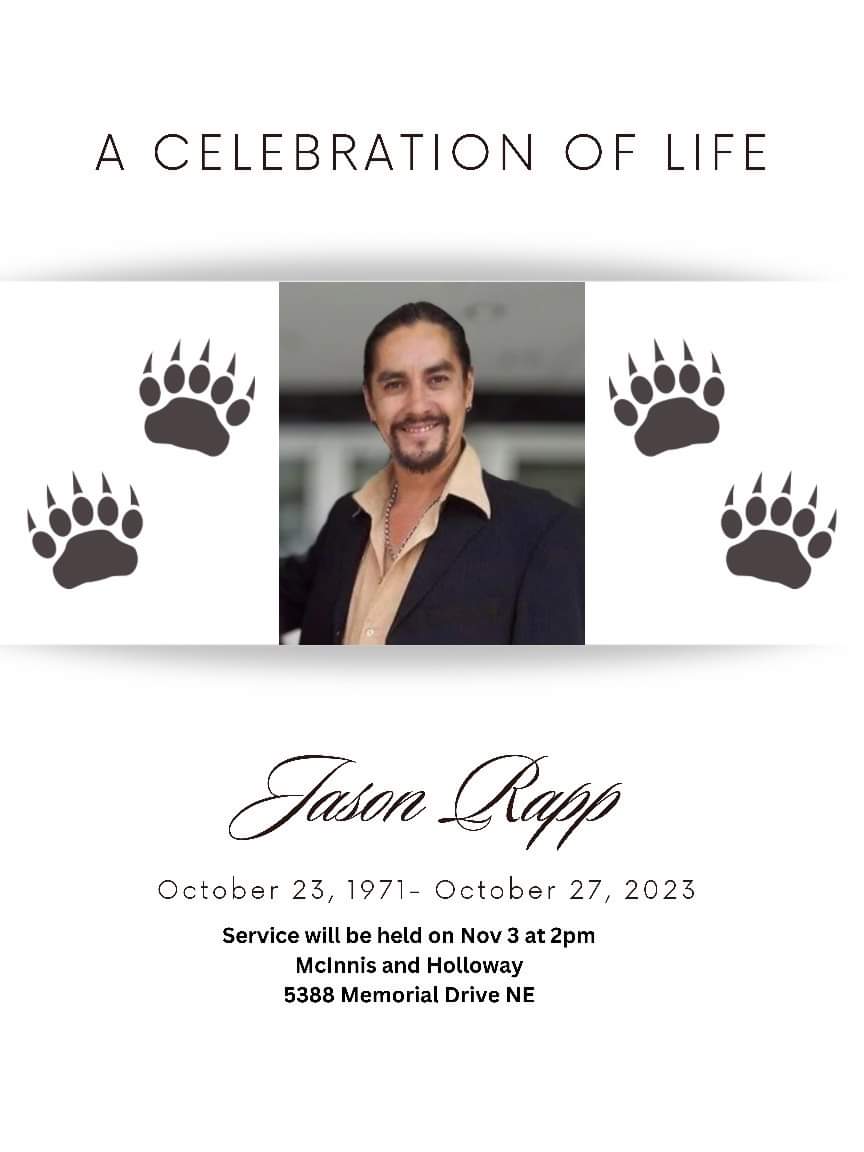
Over a year ago my first-born son posted this guitar piece on Soundcloud. It pains me to no end to listen to this and having found out that he passed away on October 27th 2023. - He was just 52 years old! His funeral is set for November 3rd 2023 in Calgary, Alberta. Jay was his nickname, in fact he went under Jay Wormbox on Facebook. Wormbox is the name of the band he was the lead guitarist. His given name is Jason Rapp. RIP my son - I love you and my heart aches. Perhaps we see each other again when I too will go over the rainbow bridge. I weep as I write this.
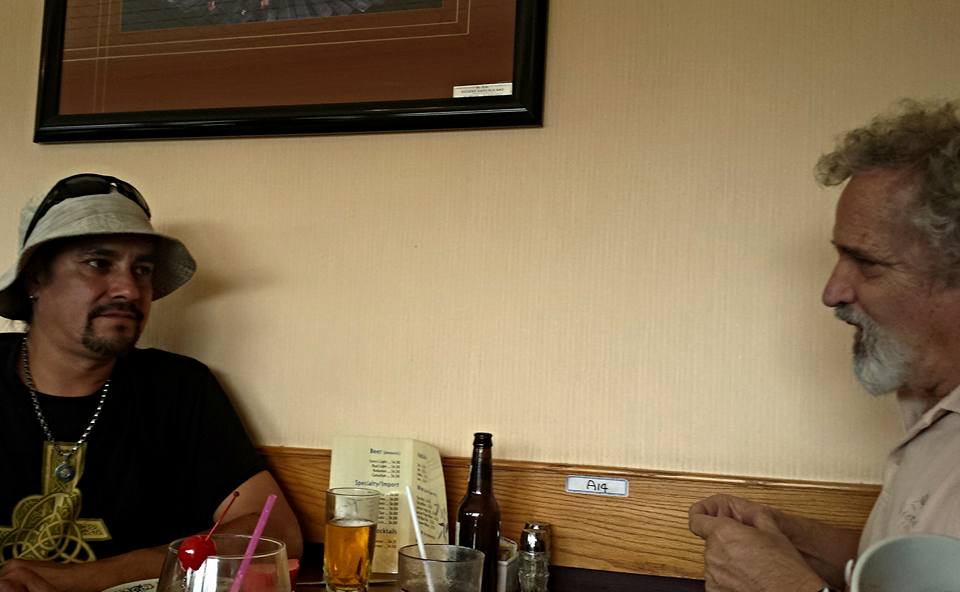
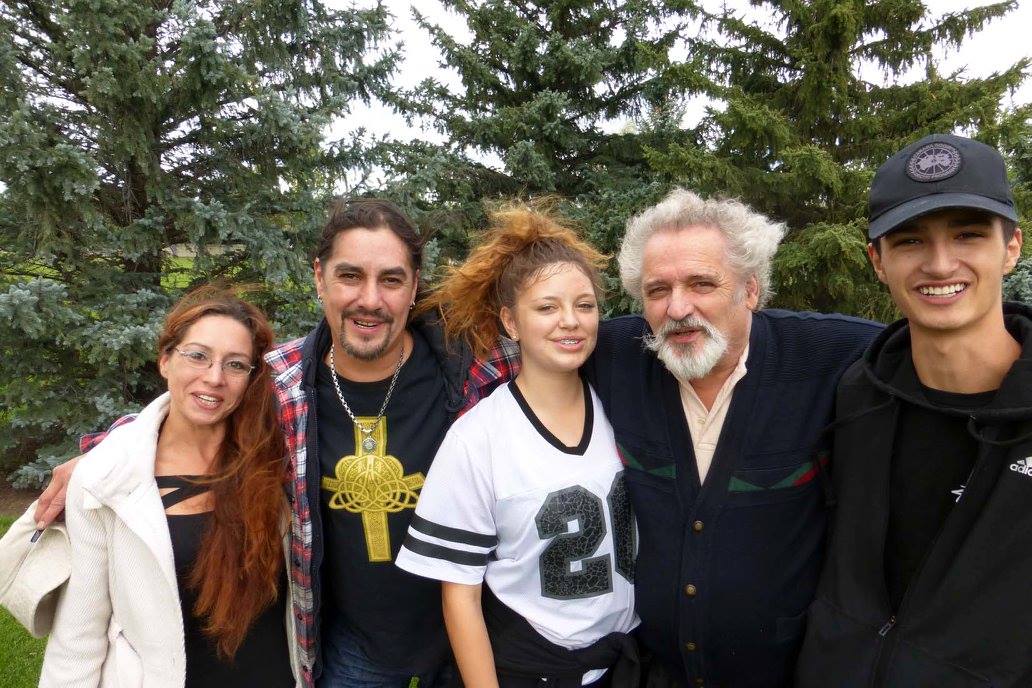
The last time I seen my son personally was 2015 in Lethbridge, Alberta, when I came for a vacation visit to my former home. He came from Calgary to see me, together with his two children Trista and Sebastian. Spending time with my younger son Otti and his mother Christan.
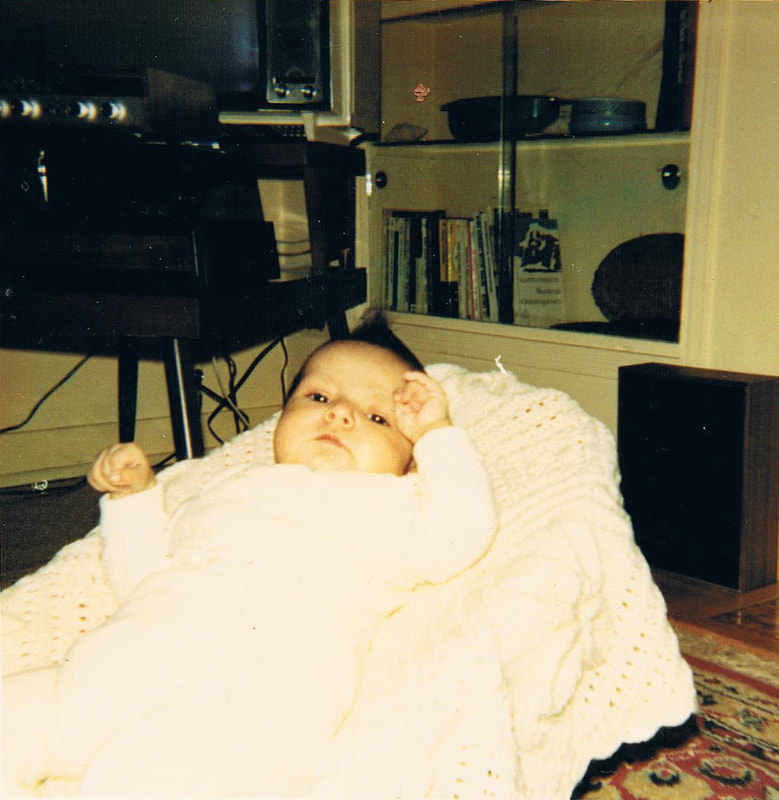
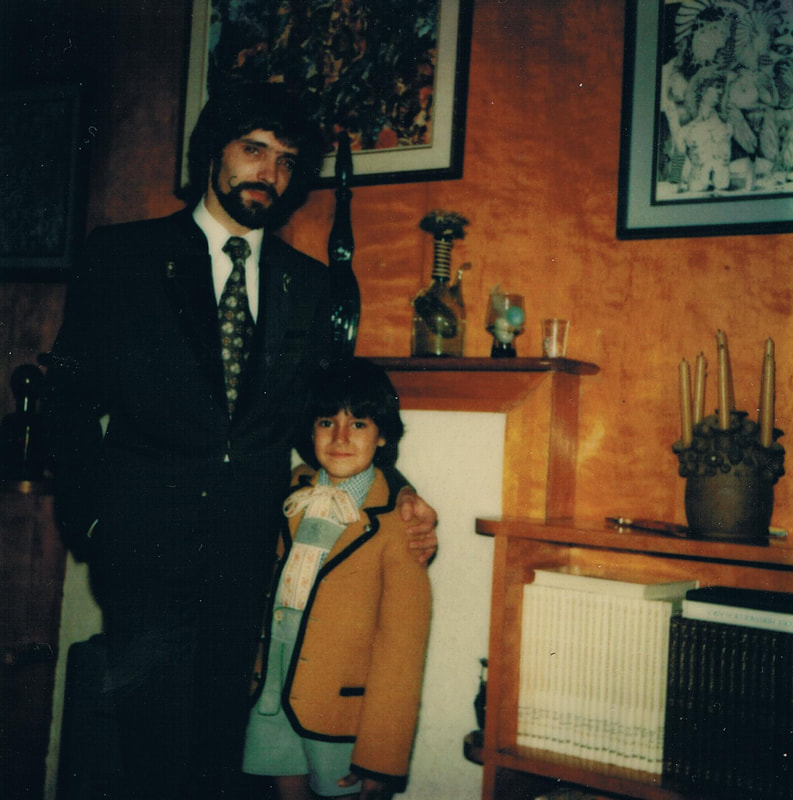
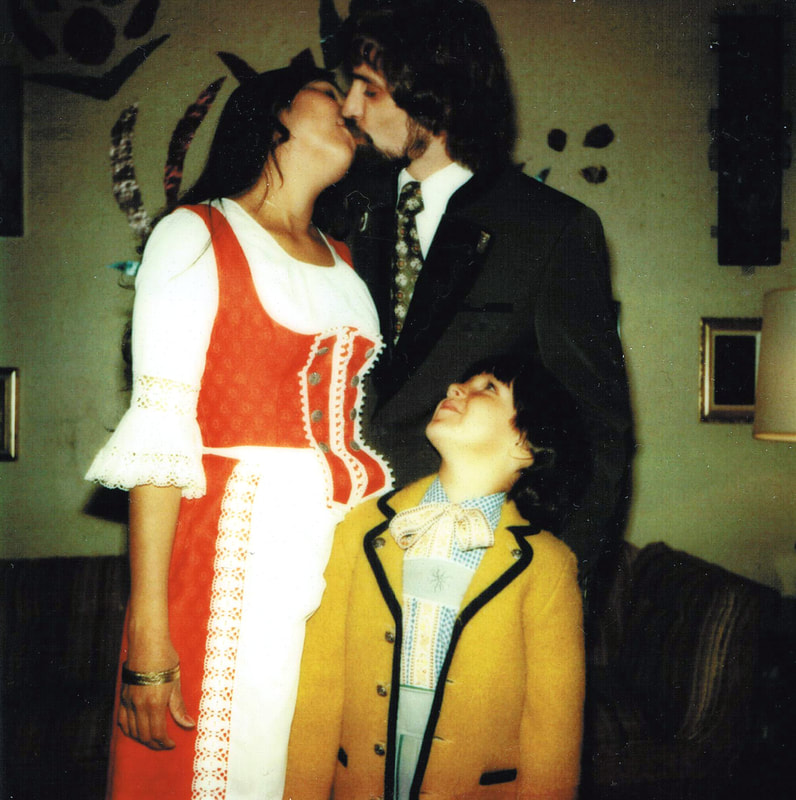
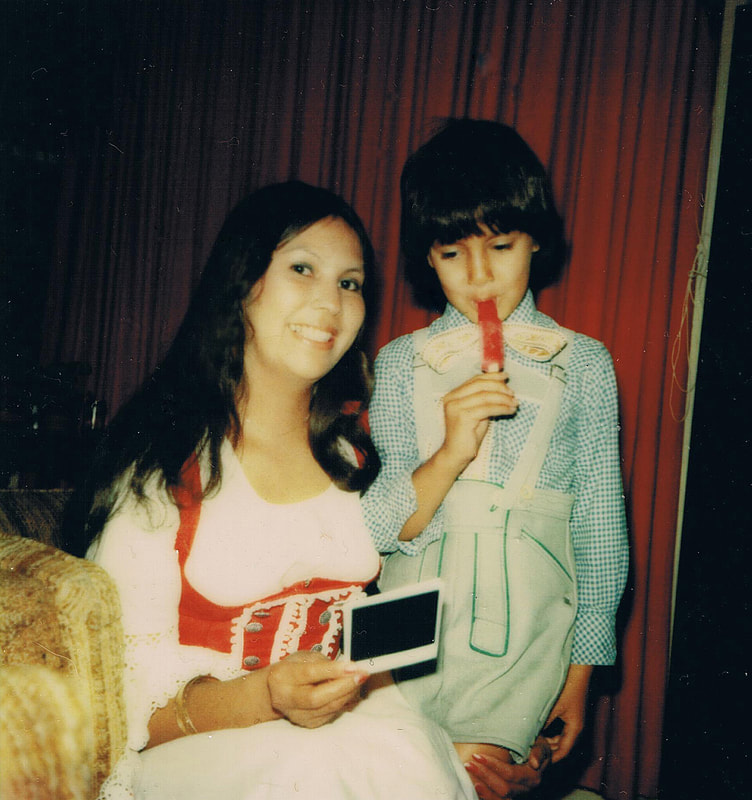
I remember as if it were yesterday, the times we had when he was just a little boy. These pictures are particularly precious to me, recovered and scanned from an old album. His mother, Mary Jane, passed away in 2009. After we separated in 1988, Mary Jane also had 2 daughters, Tasha and Nicole.
CALGARY, ALBERTA, CANADA
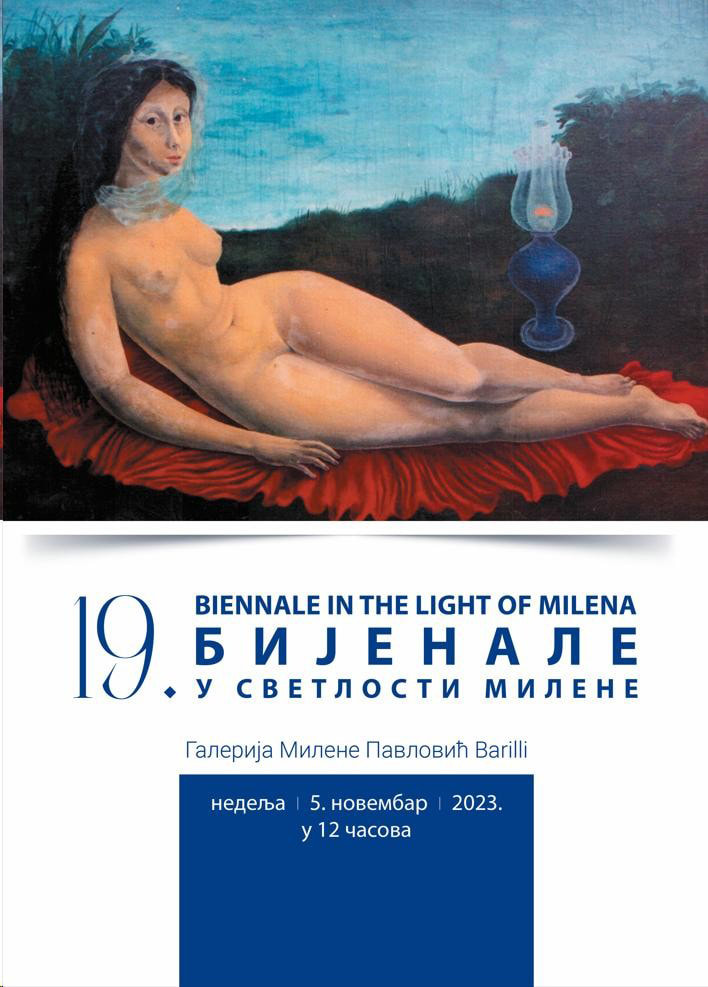
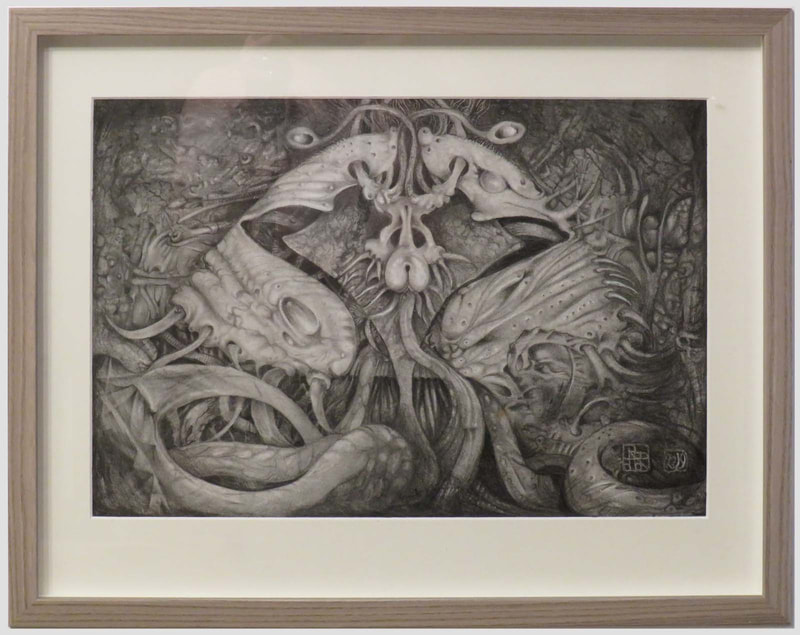
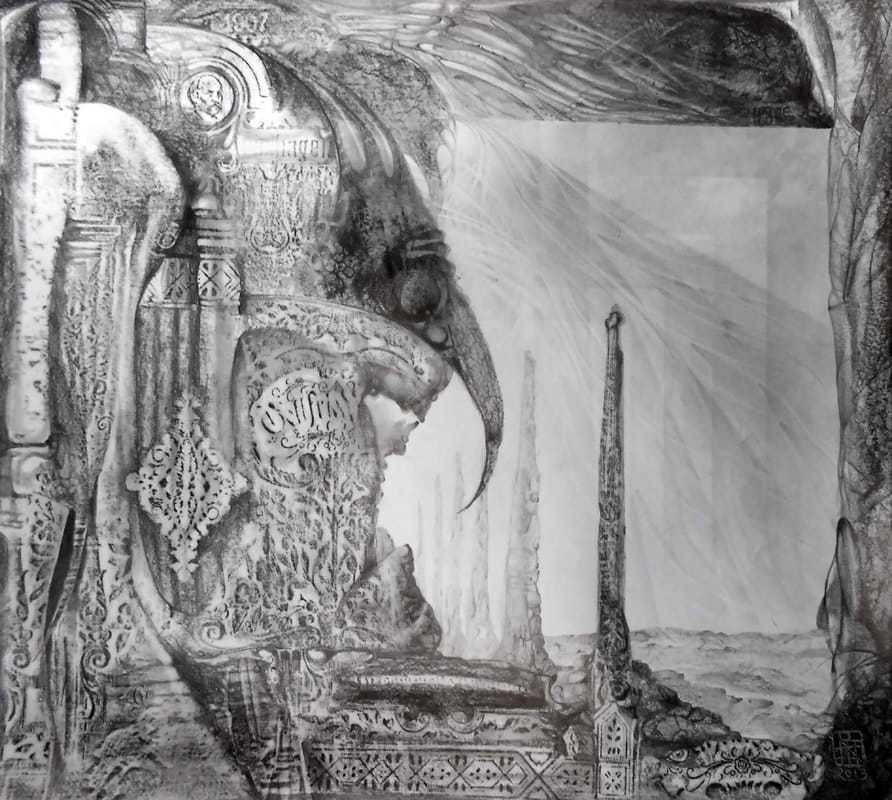
I am happy to have been selected to participate in this exhibition in honor of Serbian artist Milena Barilli I am participating in this invitational exhibition in honor of Serbian artist Milena Pavlovic Barilli with one painting and one drawing. https://www.culturalplaces.com/tour/the-gallery-of-milena-pavlovic-barilli Official opening is on November 5th, the birthday of the artist. The exhibition will be opened by Dijana Metlic, art historian, Snezana Petrovic, artist and selector for this years event, and Vladimir Dunjic, artist who won the top prize last year. Milena Pavlović Barili was one of the most prominent Serbian artists of the first half of 20th century. She was well acclaimed in artistic circles of Europe and USA. The gallery houses nice selection of here works from all the periods of her short life including posters and covers she did for Vogue, Harpers Bazaar and other famous magazines and some of her personal belongings. The gallery is open from 7 to 15h from Tue till Fri and from 8 to 16h on Sat. I am participating with these two works - both completed in 2023 - a drawing and a acrylic painting
On Saturday, October 7th 2023 my friend Artist Shahram Alizadeh opened his atelier for a group show of fantastic artists, where I had the opportunity to participate with some of my artwork. The display will be open-ended, that is, I can exchange my work with other pieces at any time. This is both Shahram's atelier as well as a showroom for his artist friends.
On Tiktok I made a vide from clips and photos that Shahram provided, adding special effects (and the 'obligatory selfie' at the end, which is a transition creation from Dreamwombo. The charcoal drawing of 'Nubian Kore' is not in the video, but it is displayed in the back room part, whereas the other two are in the front room.
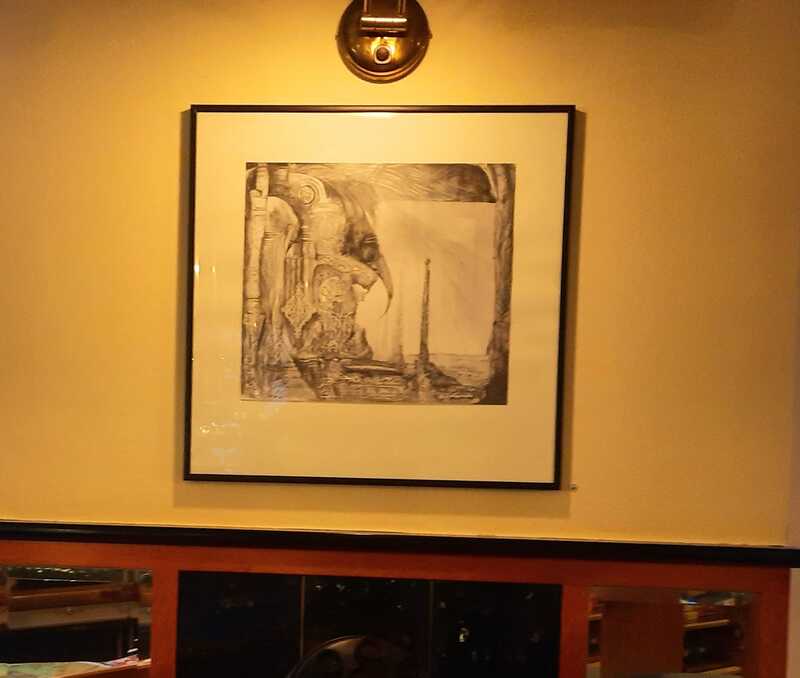
In connection with the OPEN STUDIO at the KUNSTQUARTIER WIEN MEIDLING, a selection of artwork from our house was placed at the nearby Cafe Cosmos which will be there for about two or three weeks. The Open Studio was held on September 30th 2023 and was quite a success. This was my OPEN STUDIO at the KQWM
 Yesterday I received a Email from my POD Merchandise ART OF WHERE to inform me that the associated web page for my products will not be maintained anymore after April 2023. This announcement came via Mailchimp. It is a bit frustrating - on Facebook I wrote: According to the latest update from my AOW Print-on-Demand place, the store web page will no longer be maintained after April 2023. I would have to host my own store (pages?) on my own website, or else join Etsy or Shopify to offer my products via API from AOW. All rather complicated and time-consuming work to make those changes. This is frustrating. For anyone to check out within the next few weeks, here is my existing store on the AOW website that will be no more after a month (get it while it lasts - I will still be able to sell my creations, but have to make other arrangements): MY AOW STORE PAGE ART OF THE MYSTIC OTTO RAPP After some time of being idle, I just recently created a number of items so maybe check them out while my store page is still up. Still available to order from my store page until end of April.
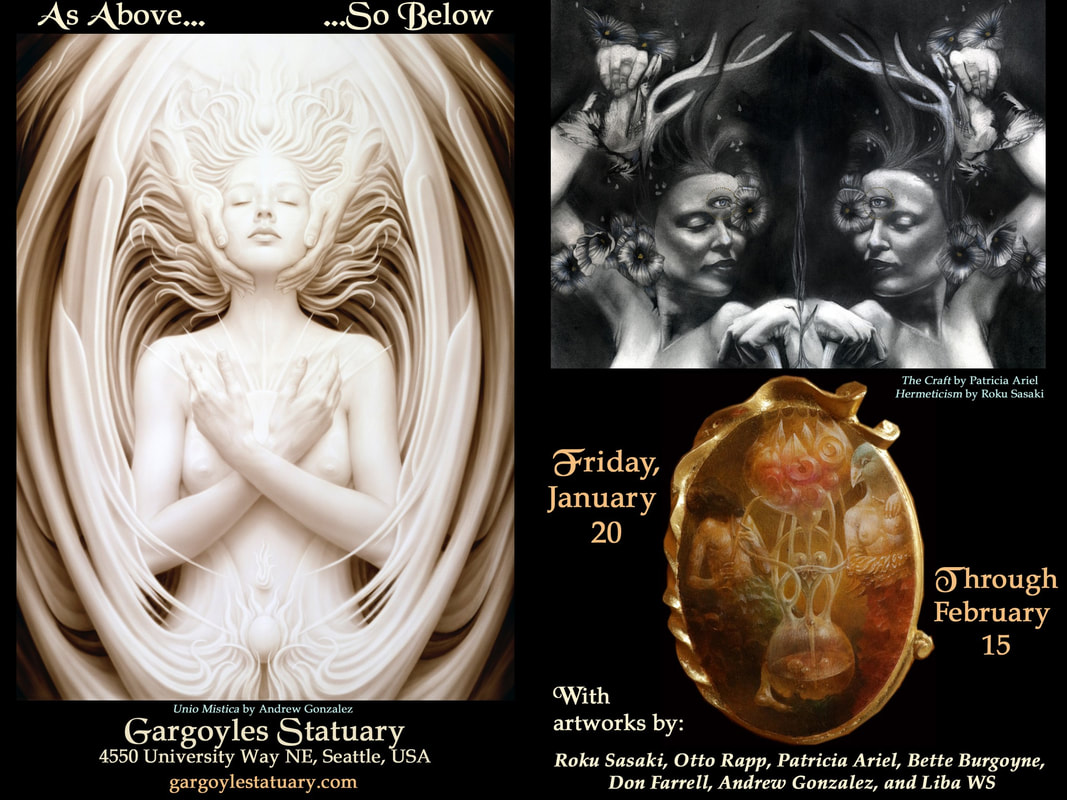
AS ABOVE - SO BELOW
After some time of low activity I am pleased that some work of mine had been chosen for a show in Seattle. This was announced by my friend Don Farrell who had on previous occasions placed works of mine that he is taking care of in shows in the Seattle area.
January 20th 2023 to February 15th 2023
https://gargoylestatuary.com/ 4550 University Way NE Seattle, WA 98105 206-632-4940
GOOGLE CALENDAR - add it to your calendar

I am posting two versions - one from YouTube Age restricted, only available directly on YouTube - but if that one gets deleted (again?) I embed one from Rumble ▼ Ukraine. Across its eastern border is Russia and to its west-Europe. For centuries, it has been at the center of a tug-of-war between powers seeking to control its rich lands and access to the Black Sea. 2014's Maidan Massacre triggered a bloody uprising that ousted president Viktor Yanukovych and painted Russia as the perpetrator by Western media. But was it? "Ukraine on Fire" by Igor Lopatonok..
2020 / 2022 - For the past two years, the world population has been under the spell of the coronavirus. Emergency regimes have been established, civil liberties have been dismantled, surveillance programs were being installed and an unprecedented global vaccination program has been rolled out.
Are we doing the right thing, or did we make a deal with the devil in exchange for a benefit? Through critical voices from various areas of expertise, PANDAMNED attempted for the first time to paint the whole picture and shed light on the darkness. It has become a relentless stocktaking of our time, which global organizations, governments and big tech companies would have preferred to prevent. Documentary maker Marijn Poels takes the viewer on an enlightening journey through the emerging absurd world of the "New Normal" and how we can still prevent it. www.pandamned.org Subtitles: German, Englisch, Dutch For my German readers, here is a excellent article in German für meine Deutschen Leser, hier ist ein sehr guter Artikel auf Deutsch über diesen Film: «Pandamned» – Dokumentation über die Hintergründe der Corona-Politik |
OTTO RAPPThis blog is primarily art related - for my photography please go to Archives
April 2024
Categories
All
|







































 RSS Feed
RSS Feed